Gut healing supplements can feel like a maze. Too many bottles, big promises, not a lot of plain talk. If you’re dealing with bloat, bathroom swings, random food reactions, or skin that will not chill, you’re not “being sensitive.” Your gut is asking for help. Let’s keep this simple, practical, and human.
What are the best supplements for gut healing?
There isn’t one hero capsule. There’s a small crew that tends to help—if you match them to your symptoms and give them time.
Probiotics are the quiet nudge. A solid multi-strain with Lactobacillus and Bifidobacterium often means less gas, better rhythm, and a calmer immune tone. Super reactive? Start with spore‑based (Bacillus). Pinch‑of‑a‑dose. Hold steady for 6–8 weeks.
Prebiotics are food for your good bugs. PHGG (partially hydrolyzed guar gum) is usually the gentlest. Acacia is soft on a fussy belly, too. Inulin and GOS can work—just micro‑dose and pace yourself if you bloat easily.
Postbiotics give the lining direct love. Butyrate or tributyrin helps tighten the barrier, soothe irritation, and can settle loose, urgent stools.
Digestive support takes the weight off your stomach. A broad enzyme with your first bite can help if meals just sit there, or you see undigested food. Betaine HCl is sometimes used when stomach acid is low—but not with active gastritis, ulcers, or a reflux flare. When in doubt, skip it or get guidance.
Mucosal soothers are the repair crew. L‑glutamine plus zinc carnosine is a classic combo for tenderness, post-infection irritability, or stressy flares. DGL, aloe inner fillet, slippery elm, and marshmallow root can provide comfort.
Targeted antimicrobials are tools, not a lifestyle. Berberine, oregano, neem, allicin—short, guided cycles only, then rebuild with probiotics and prebiotics. Too much “kill” and not enough “rebuild” makes recovery drag.
Polyphenols are the background helpers. Pomegranate, green tea catechins, cranberry—they quietly nudge your microbiome and support the lining.
If hormones tend to kick up gut drama (PMS, acne, irregular cycles), this is a helpful mid-read context from The Hormone Nest: Premenstrual Syndrome PMS Treatment That Feels Human – Real Relief.
A quick personal story
A couple of summers ago, I could set my watch by the 5 p.m. bloat. Breakfast? Fine. Lunch? Dicey. Late afternoon? Balloon animal. I cut dairy, then gluten, then joy. I rotated probiotics like socks. It helped, then didn’t.
What finally worked was not flashy. I started a spore‑based probiotic—just a dusting. Added PHGG at a quarter teaspoon and waited. L‑glutamine with zinc carnosine first thing, away from food. Two weeks in, the 5 p.m. swell slid from “ugh” to “manageable.” Week six, my bowels remembered they like a rhythm. Not perfect—just human. That’s the win most of us actually need.
Do probiotics actually heal the gut?
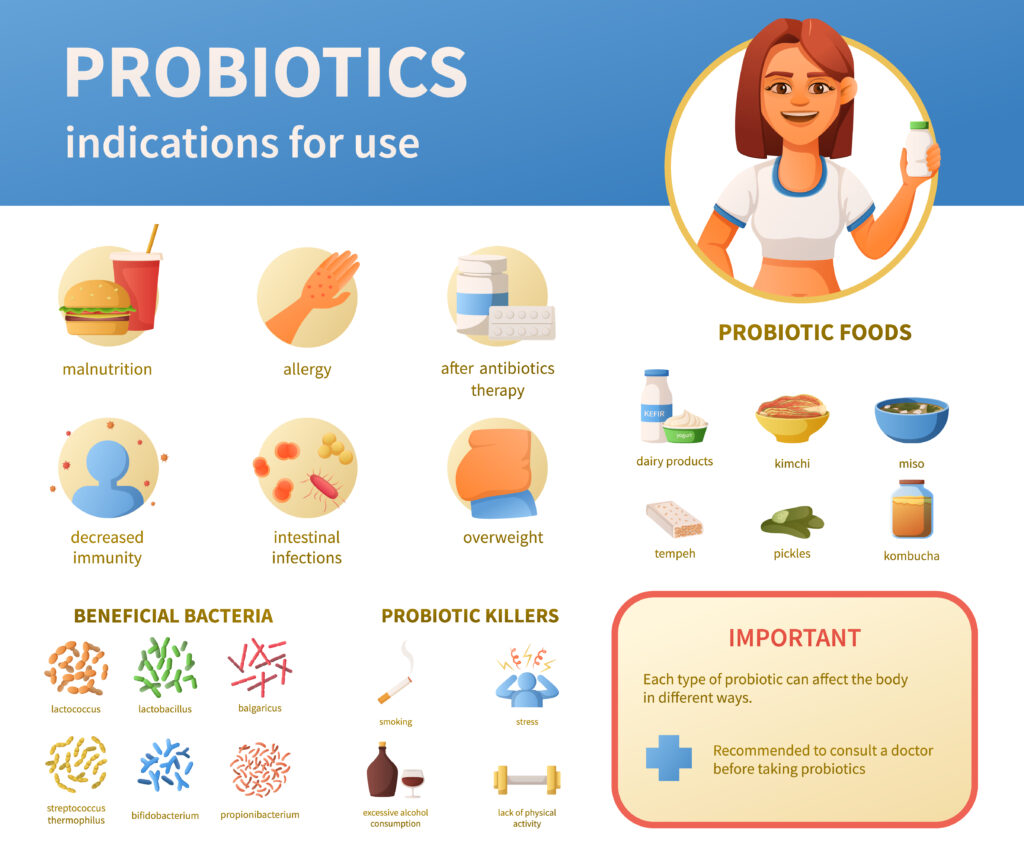
They don’t move in forever. But while you take them, they crowd out troublemakers, make short-chain fatty acids that feed your lining, and nudge the immune system away from high alert. Many people see less gas and steadier mornings.
Sensitive folks: start with crumbs. Spore‑based or a tiny multi‑strain dose. Give it 6–8 weeks. Track three simple things: bloat (0–10), stool form (Bristol chart), and post‑meal energy. Your notes tell the truth better than any label.
Is L-glutamine good for “leaky gut”?
Short answer: yes. L-glutamine fuels the cells that line your intestines and supports the tight junctions between them. Common dose: 3–10 g per day, split, away from meals. If things slow down at higher doses, step back, then retitrate. Pair with zinc carnosine if you’ve got lingering tenderness, reflux, or post‑infection irritation.
Which fiber is best for bloating?
It depends on your baseline and how reactive you are. PHGG is often the easiest for IBS-ish bloat and mixed stools. Acacia is a close second if inulin has betrayed you before. Inulin and GOS can be great—just start tiny. Psyllium helps stool form but demands hydration.
Rule of thumb: start at a quarter to half serving. Sit there for 3–5 days. Then nudge up. Consistency beats hero doses.
Do digestive enzymes and HCl help with gas and heaviness?
If meals camp out in your stomach, you burp a lot, or you spot undigested food, a comprehensive enzyme with the first bite can lighten the load. Full fast, constant burps, long‑term acid blockers in your history? Low stomach acid could be in the mix. Some people trial betaine HCl—never with active gastritis, ulcers, GERD, or on acid blockers. Pale or floating stools? You may need bile support under guidance. These are targeted tools, not forever supplements.
What is butyrate, and why is it popular?
Butyrate is a short‑chain fatty acid your microbes make when they ferment fiber. It’s fuel for colon cells, supports barrier integrity, calms inflammation, and helps motility. People reach for it (or tributyrin, which smells less) when stools are loose or urgent, or when the colon feels cranky. If it makes you queasy, take it with meals.
Are antimicrobial herbs necessary for gut healing?
Usually, no. Save them for documented or very likely overgrowths. If you use them, keep them short and structured. During a protocol, support motility (ginger, light movement, magnesium) and bile flow (bitters, lemon/olive oil). Then rebuild. Overdoing antimicrobials is like pulling weeds and never re‑planting—bare dirt doesn’t stay bare.
How long does it take to heal the gut?
It depends—history matters. Food poisoning, infections, stress, hormones, meds, autoimmunity—all change timelines. Rough sketch:
Some relief in 2–6 weeks if the stack fits. Deeper remodelling of the lining and microbiome: 8–16+ weeks. Maintenance looks boring in the best way: decent sleep, enough protein, colourful plants, gentle movement, stress care, sunshine. Think in phases: calm and soothe; normalize digestion and motility; re‑introduce fibers and diversity; then keep a minimal, sustainable routine.
Can I take multiple gut supplements together?
Yes—but layer. Start with L‑glutamine, zinc carnosine, and a gentle probiotic. After two weeks, add PHGG. Still loose? Bring in butyrate. Heaviness after meals? Add a broad enzyme. If testing shows overgrowths, do a short antimicrobial phase with guidance, then rebuild. Adjust by trends, not single days.
What foods should I pair with supplements for the best results?

Keep meals steady and kind. Anchor protein at each meal (roughly 20–35 g). Start with cooked veg if big raw salads puff you up. Use colour and herbs like tools—berries, olive oil, oregano, thyme, turmeric, and cocoa. Begin with gentler carbs—white rice, well-cooked oats, ripe bananas—then expand to beans and whole grains as you tolerate them. Hydrate. Magnesium glycinate or citrate can help motility; electrolytes help if stools run loose.
Greece‑friendly tweaks? Thick Greek yogurt or kefir if tolerated, feta in small amounts, extra‑virgin olive oil on basically everything, lemon and oregano on grilled chicken or chickpeas, and ripe tomatoes/cucumber in smaller portions if raw veg has been touchy.
If hormones play in, fiber timing and seed cycling can smooth things out. Near the end of your plan, this companion read from The Hormone Nest is handy: Cycle Syncing Diet for Hormonal Balance.
Example day: timing, quantities, meals
This is a sample day—tweak portions and foods for your body and culture.
7:00
Water with a pinch of sea salt and lemon. L‑glutamine 5 g + zinc carnosine as labelled, away from food.
7:30 Breakfast
Greek-style omelette: 2–3 eggs, spinach, zucchini, and fresh dill in olive oil. Or well-cooked oats with cinnamon and a drizzle of tahini. Gentle probiotic with the first bites.
10:30 Mid-morning
PHGG ¼ tsp in water. If fine after three days, increase to ½ tsp. A handful of strawberries or blueberries.
13:30 Lunch
Grilled chicken or chickpeas with lemon and oregano, olive oil over steamed carrots and green beans. A small serving of white rice or boiled potatoes. If meals feel heavy, take a comprehensive digestive enzyme with the first bite.
16:30 Snack
Plain Greek yogurt or kefir if tolerated (or lactose-free). A few walnuts. Ginger tea for motility.
19:30 Dinner
Baked salmon or sardines with olive oil and lemon. Roasted eggplant and red peppers. Small Greek salad (cucumber, tomato) if raw veg is okay; if not, keep most veg cooked. If stools are loose, take tributyrin or butyrate with the meal.
21:30 Evening
Magnesium glycinate 200–300 mg if constipation-prone. Chamomile tea. Short walk or gentle stretch.
Sunday check-in
Note your week: average bloat, stool form, energy after meals. If steady, nudge PHGG up by ¼ tsp. If loose stools persist, keep butyrate for another 1–2 weeks, then reassess. Plateau at week six? Rotate probiotic strains or expand fiber diversity.
What’s the simplest “starter” protocol?
Six to eight weeks. Minimal stack. Morning, away from food: L‑glutamine 3–5 g + zinc carnosine. With breakfast: gentle probiotic (spore‑based if super sensitive). With lunch or dinner: PHGG or acacia, starting ¼–½ tsp and creeping up slowly. Optional: a broad enzyme at your biggest meal; butyrate if stools are loose. Week six: reassess and adjust.
References
Gibson, G.R., et al. (2017). Expert consensus: The concept of “prebiotics.” Nature Reviews Gastroenterology & Hepatology
McFarland, L.V. (2015). From yaks to yogurt: probiotics and their fermented food vehicles. Microorganisms
Zhang, M., et al. (2016). Butyrate: A gut microbiota metabolite regulating intestinal function. Trends in Endocrinology and Metabolism
Iovino, P., et al. (2023). Partially hydrolyzed guar gum in IBS: A review. Nutrients
Vanuytsel, T., et al. (2014). Zinc carnosine and mucosal protection. Gut
Disclaimer: This article is educational and not medical advice. Always consult your healthcare provider before starting or changing supplements, especially if you have medical conditions, take prescription medications, are pregnant or breastfeeding, or have ongoing GI symptoms.








